Kobro's Cancer Crew #5: Treatment Day
Hey David, our last update covered some good news. I have Classic Hodgkin's Lymphoma which is the most curable type. It's still stage 4, but tomato tomaahto.
This update covers my first day of treatment and all the drugs involved.
Fun aside -- I received a threat the other day.
In my last update, I shared the mean april fools joke I pulled on Mikayla (saying that the diagnosis was worse than it actually is). Aunt Nancy told me:
"And if you ever do that to Mikayla again, no more cookies for you!!!"
April 2nd
8:00am
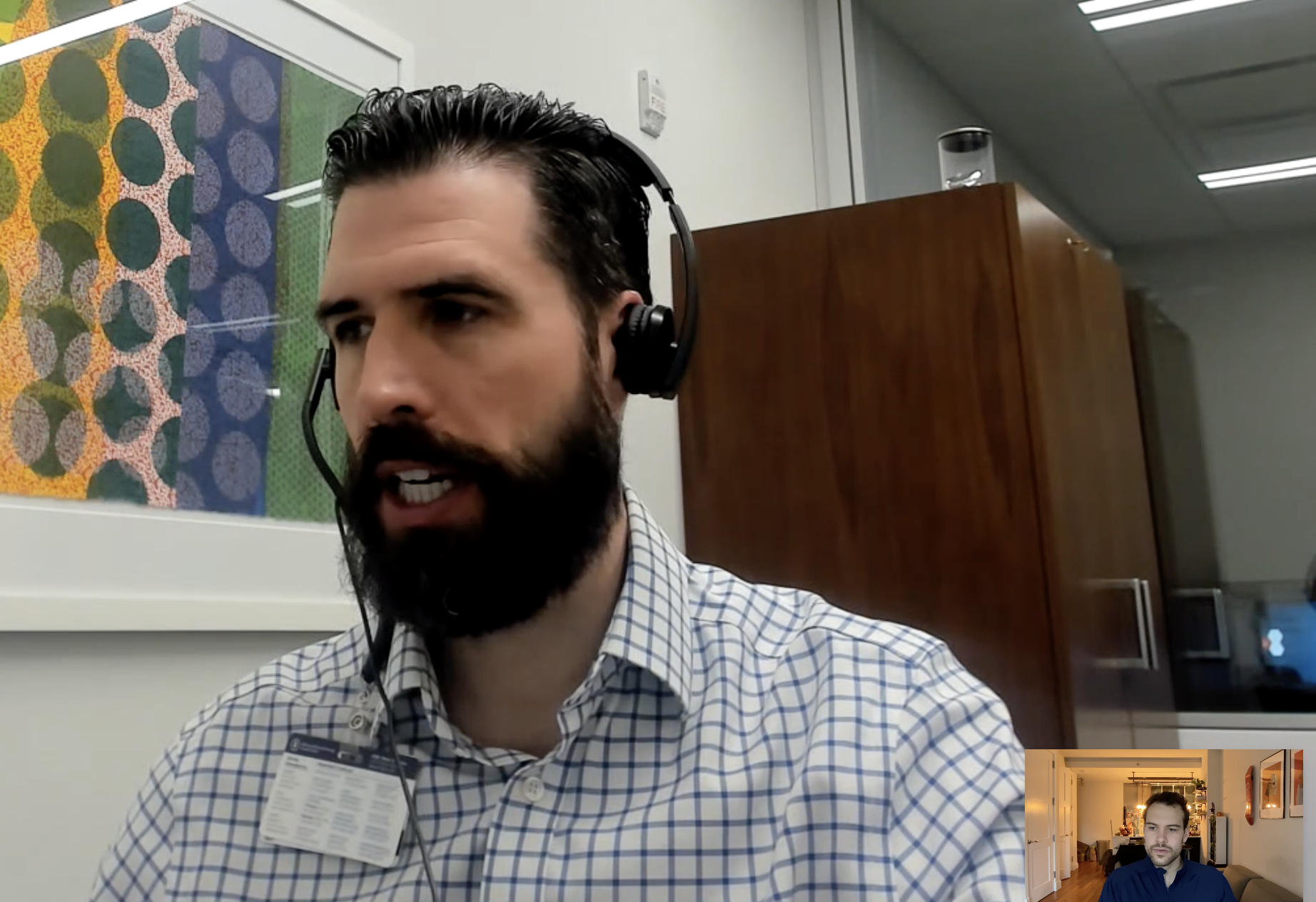
Dr. Handsome Raphael Steiner and I have a virtual checkin to make sure I'm ready to go.
We discuss how my symptoms have gotten worse over the past few weeks.
It's the first time I've had shortness of breath and consistent coughing. He comments: "That's what happens when you have a tumor pressing against your airways."
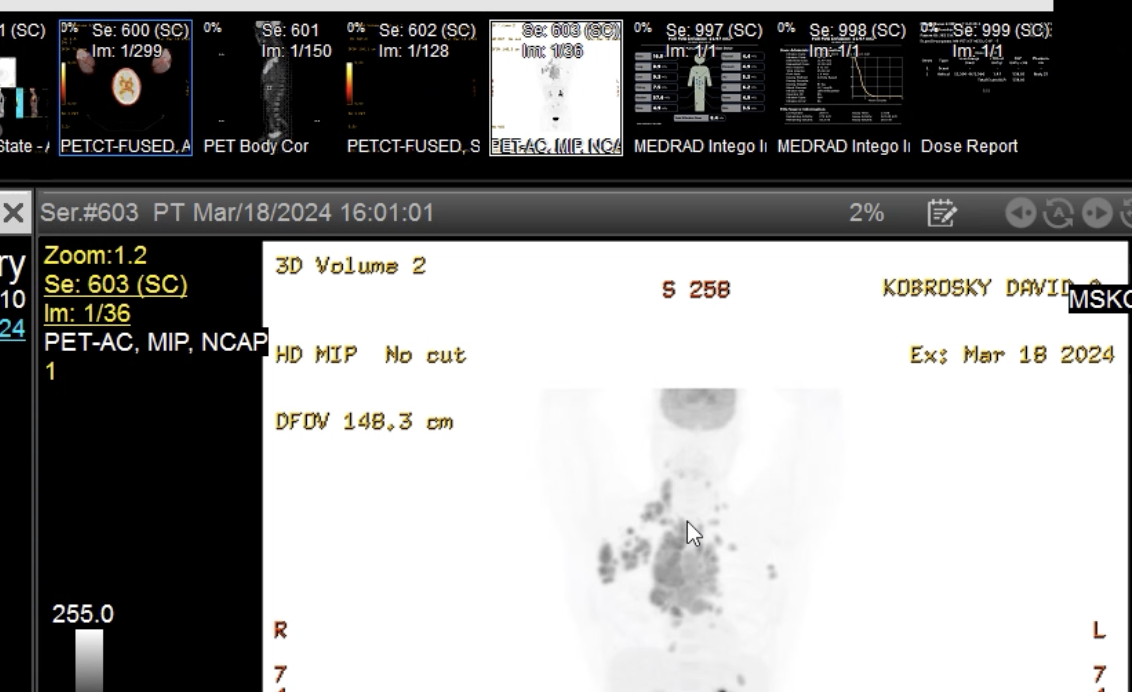
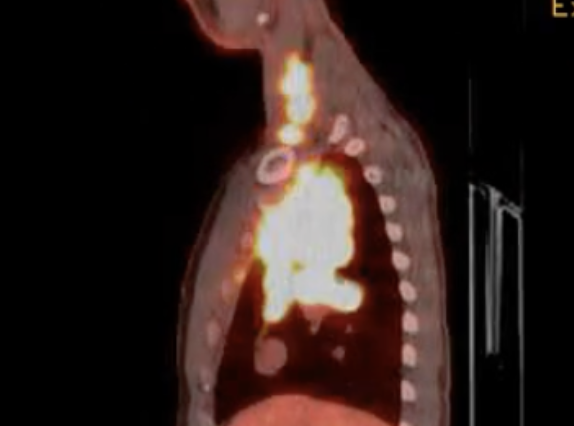
He pulls up some pictures as a reminder.
Thanks Doc, but the pictures weren't necessary ... I can feel it fine enough.
I'm officially off Zoloft! (Antidepressent / OCD drug).
You might remember from a previous update how we thought my itching could be OCD. I started on Zoloft back in January to treat the OCD, but then we learned it was cancer causing the itching.
Since then, I started weening off the Zoloft, and now we're antidepressent-free.
Finally, we get into business: I ask logistically how I can get work done during chemo - is there a desk or something? Chemo takes around 4 hours and these are precious working hours.
He says: "I'm not saying your work isn't important, but in this case ...?" He does one of those "balancing a scale" hand motions to signify that health is more important.
I told him that I'd go crazy if I couldn't work, so health and work are related to each other.
He shrugged with a "to each their own" type of look and said they have a mini desk I can use.
Tupperware takes a pen off my desk and starts chewing on it. I tell him "No" and take it away.
Doctor Handsome says, "Maybe he's a writer".
So now he's funny too 🙄.
12:00pm
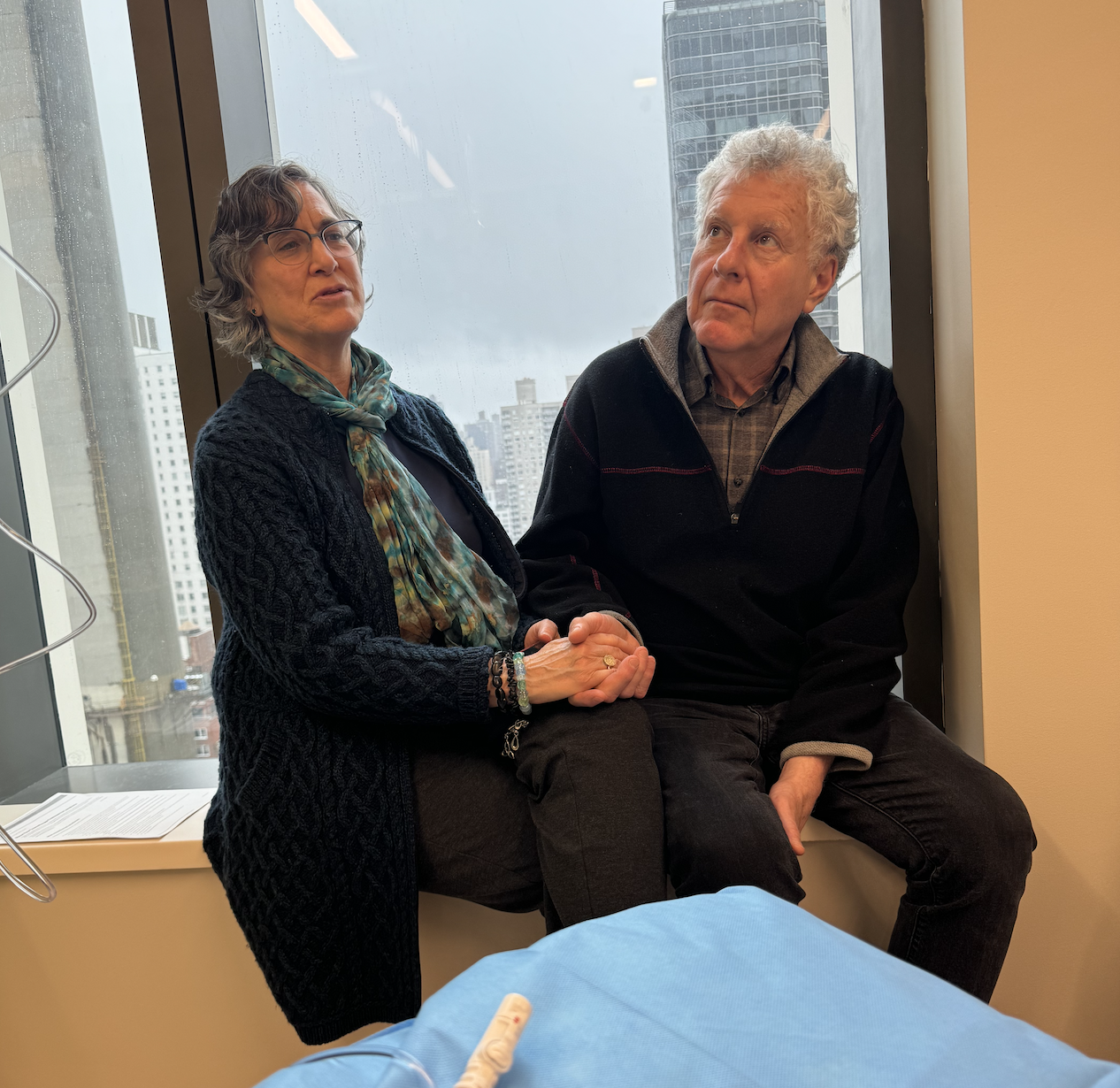
Mom & Dad fly in for the day. It's the first time Dad sees our apartment and he's impressed (primarily because of Mikayla's design choices).


I have a few work calls that morning, so I get those out of the way before we head to the hospital.
2:00pm
Once we get there, I need to get my blood drawn (they do this before each infusion).

40 second video clip -- you can tell they're keeping things together.
We end up needing to wait an extra 2 hours because there's not enough nurses on duty. We're all "itching" to get this over with ;)
Finally, one of the care coordinators leads us to our room.
5:00pm
My company's advisor and I had a call, but he told me to get back to treatment.
Finally, the nurse comes in, almost out of breath. She stumbles on a few words and says: "Sorry, my brain isn't working, just got back from lunch".

First of all, it's 5:00pm ... that's an early dinner, not a lunch.
Second, those are not the words you want to hear before your first round of chemo.
It turned out she's a fantastic nurse, but I wouldn't say it was the most reassuring first impression.
My Dad (a doctor) shows the nurse this pen.
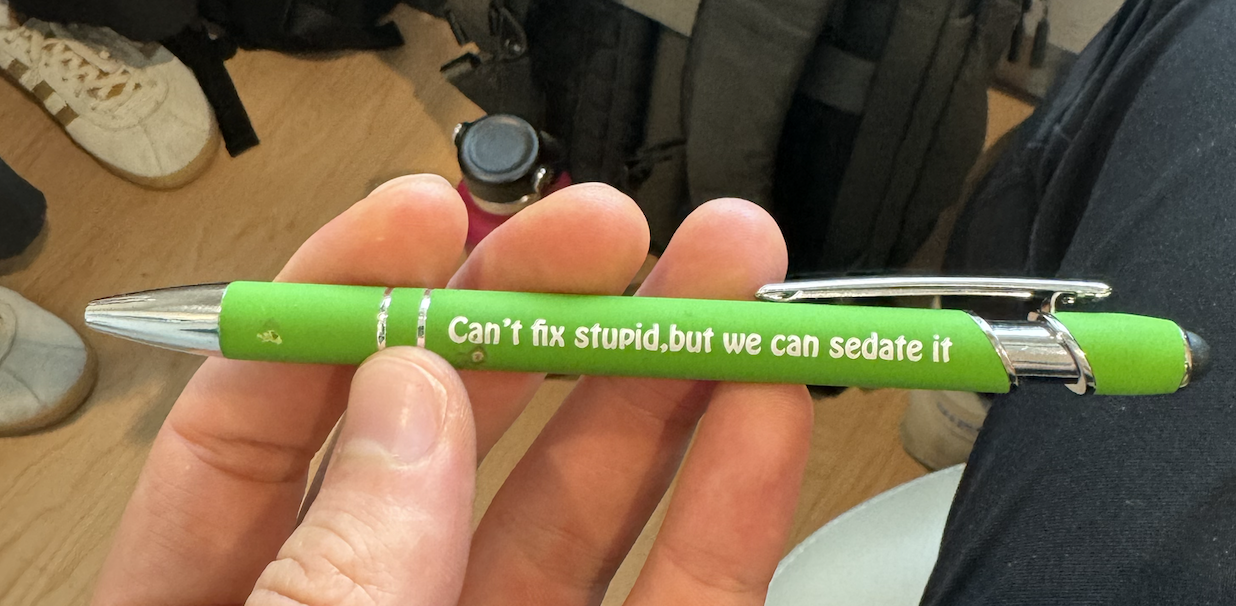
She asks my dad what type of doctor he is. He responds (for the 10,000th time): "A good one".
5:15pm
Now, quick aside before we get into the treatment: let's talk about why I need to do chemo vs. other options out there.
Right off the bat, radiation is out of the question. Since I have a large tumor bigger than an orange right next to my heart (All that bright area is Lymphoma), it would be too risky to use radiation.
Surgery also wouldn't make a difference, because there's a whole lot of cancer.
With radiation & surgery off the table it leaves us with ... drum roll please... Chemo!
Types of Chemo
It turns out there's around 50 "mainstream" chemo drugs. So it's all about making the right "chemo cocktail" as they say.
Some chemo drugs make you lose your hair, others make everything taste like metal, and yet others make your pee turn red. Side effects are the name of the game.
Generally speaking, stage 3-4 Hodgkins Lymphoma has at least 3 of the same chemo drugs with one wildcard based on the stage (and what insurance is willing to cover).
We'll cover each of these drugs in the order I took them.
5:30pm
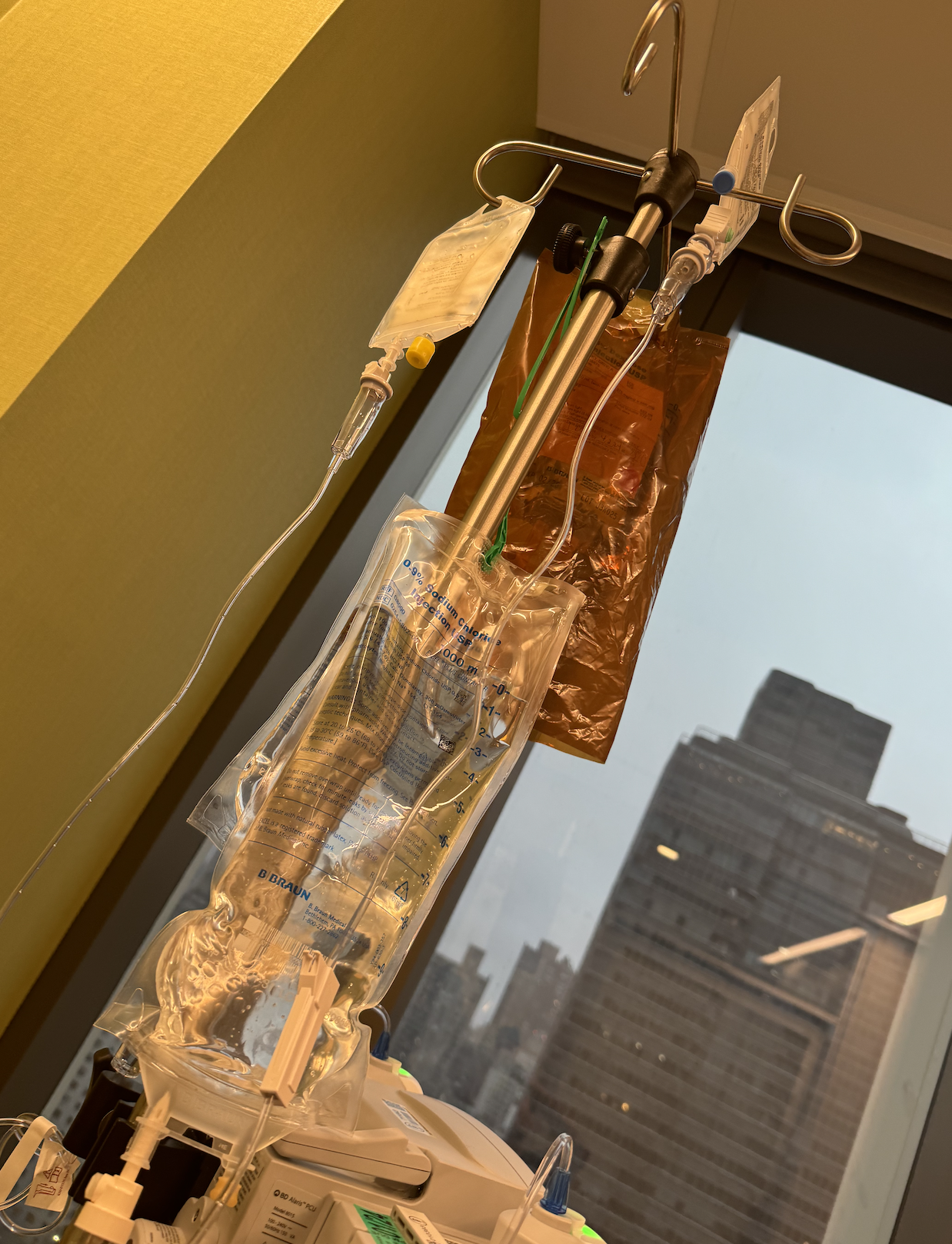
The first two things I got put in me weren't chemo, but pre-treatment nausea medicine.
The first one felt cold in my veins -- it just came out of the fridge apparently

The second one was crazy.
About 5 seconds after she started, I tasted a banana, but like a plastic banana.
A few minutes later, things got serious. Chemo time.
My nurse put on a large gown of sorts to protect her against the potential exposure.
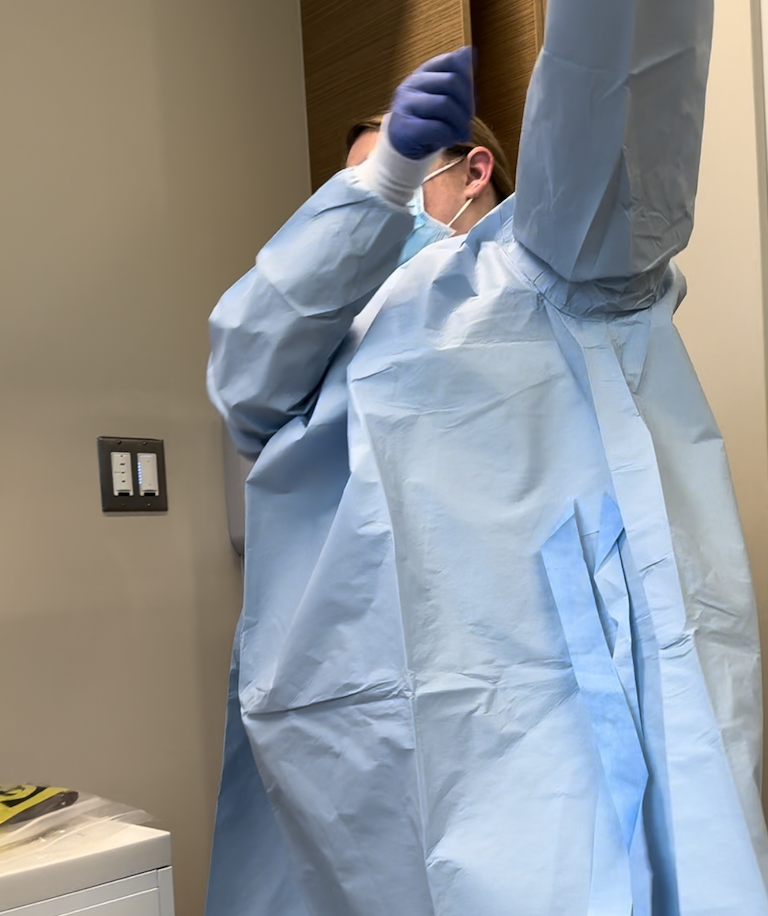
Mikayla started playing Eye of The Tiger (our friend Megan had the initial idea). Dad closed the door out of embarrassment
Here's the awkward 13-second clip.
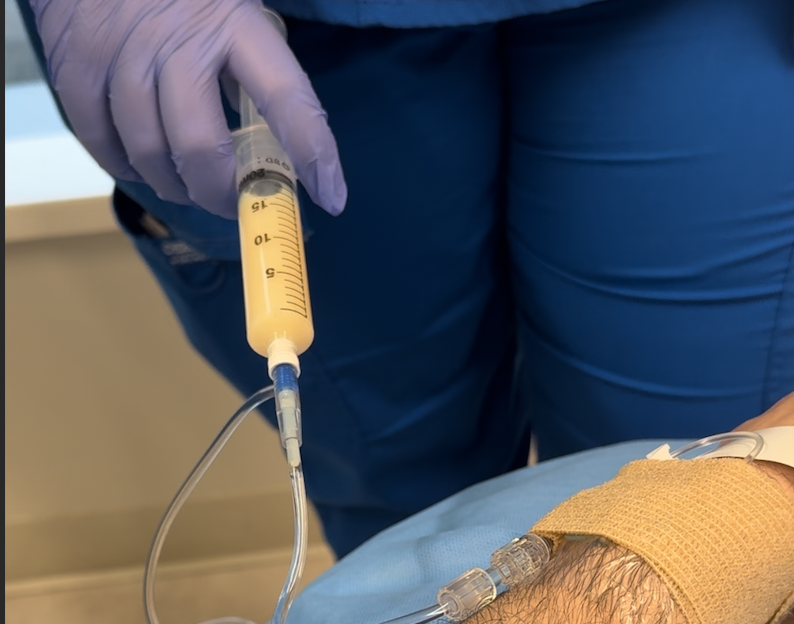
Doxorubicin (AKA Red Death -- not kidding this is the nickname)
Why I need this: Slows or stops the growth of cancer cells by blocking an enzyme that they need to divide and grow. It's considered one of the strongest drugs for breast cancer as well.
Fun fact: Doxorubicin is also known as "Red Death" or "The Red Devil" because it is a clear bright red color. It will turn my pee, sweat and tears red so I need to make sure to wear dark shirts (it stains).
Potential side effects:
- Fatigue
- Alopecia
- Nausea and vomiting
- Oral sores
- Bone marrow suppression and an increased risk of secondary malignancy diagnoses may occur.

Part of the procedure is they need another nurse to come in and verify that they're administering the correct drug into the correct patient.
Imagine how bad that would be if someone just accidentally got a dose of chemo. I asked if this happened before and they didn't have a clear answer. Not on their watch though!

Mom and Dad are having a blast.
This one felt pretty normal -- I didn't taste banana or anything out of the ordinary.
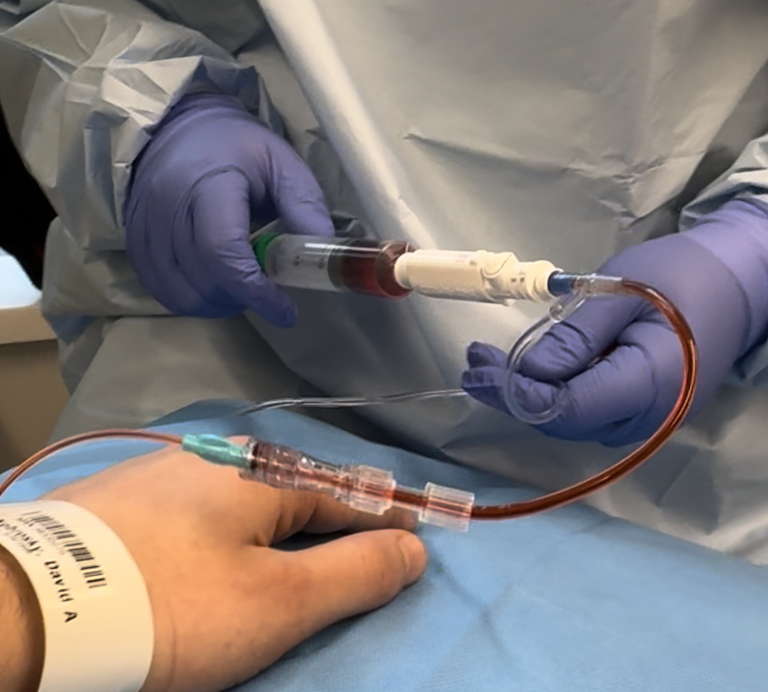
That red color is the drug, not my blood. Sorta spooky looking.
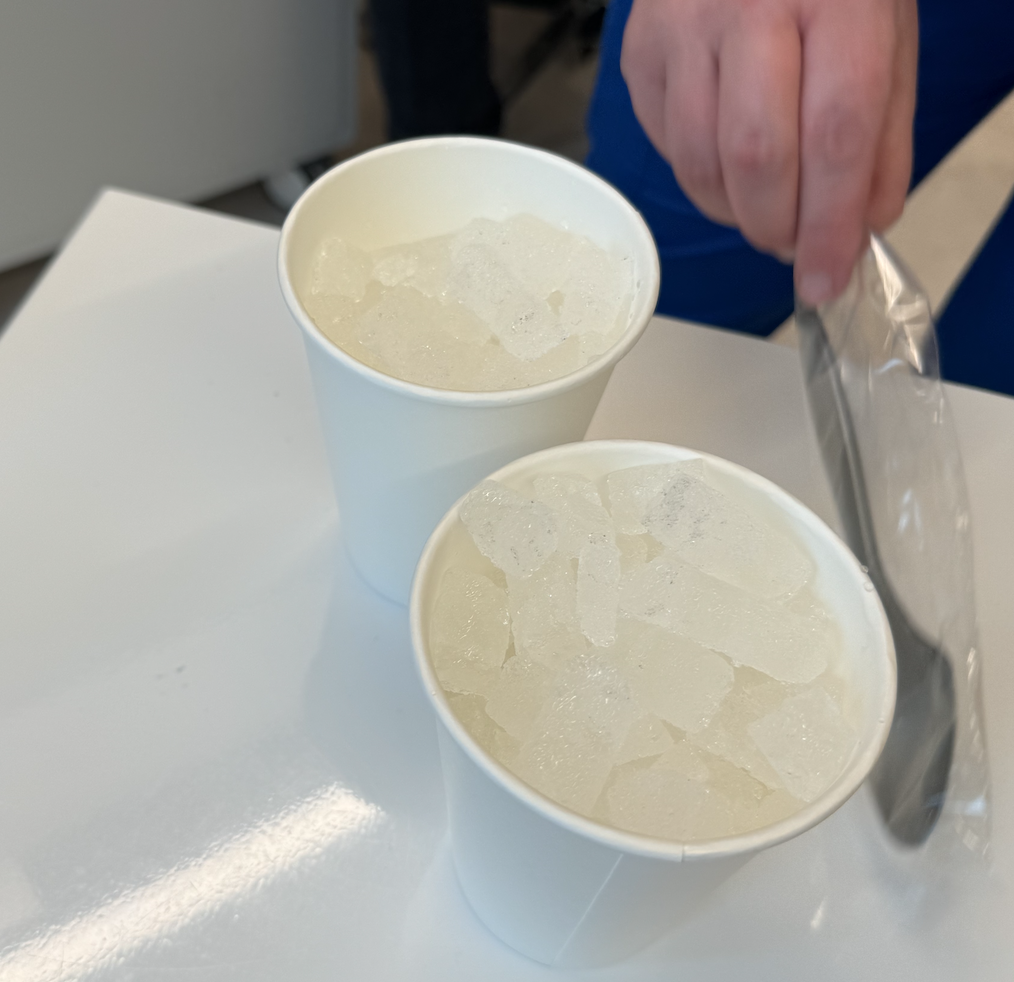
While the Red Death was doing it's thing, I was given ice to chew on.
By cooling down your mouth, apparently it keeps the chemo away from that area during the treatment. It also numbs the mouth and prevents a metallic taste.
One down, three to go!
6:00pm
Next up we had Vinblastine. Thankfully this one does not have a nickname like human destroyer or unforgiving demon.
Why I need this: Blocks cell growth by stopping mitosis (cell division).
Fun fact: Vinblastine is the salt of an alkaloid extracted from Vinca rosea Linn., a common flowering herb known as the periwinkle.
Potential side effects:
- High blood pressure which may cause headaches, dizziness, blurred vision.
- Infection, especially when white blood cell count is low.
- Anemia which may cause tiredness, or may require transfusion.
- Bruising, bleeding.
- Pain in the bones, jaw, and at the tumor.
- Constipation.
- Tiredness.
- Hair loss.
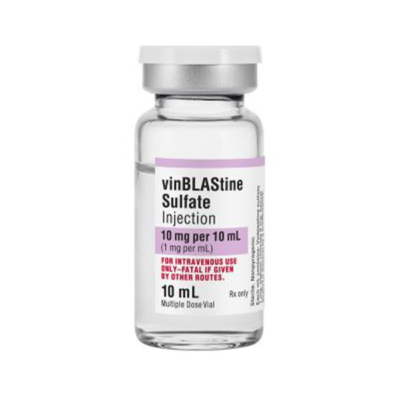
I'm losing my hair anyways, so not a big deal on the hair loss.
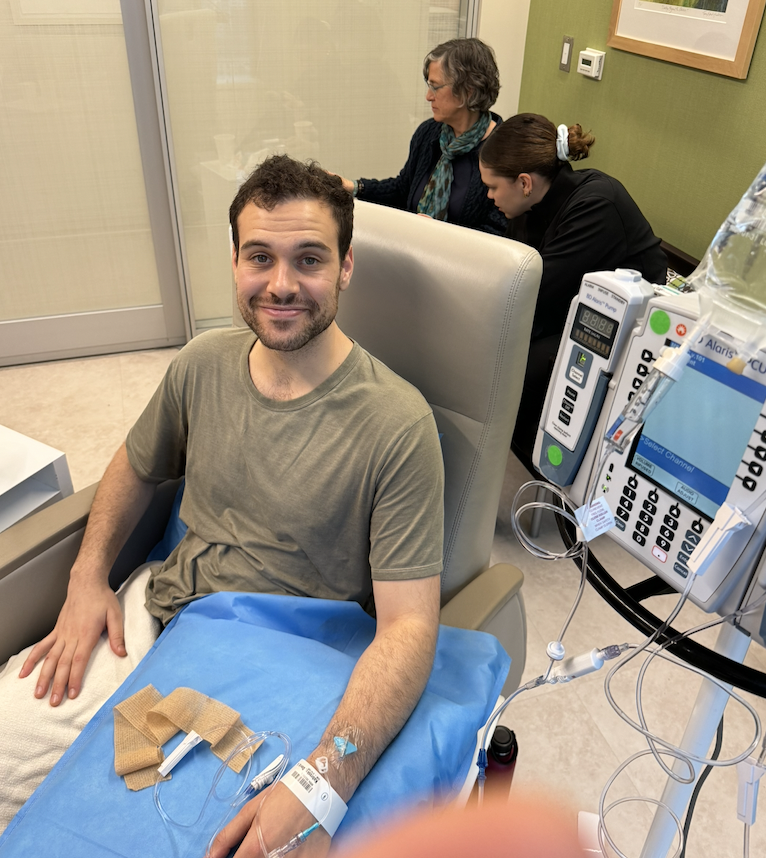
This one was easy money, took like 10 minutes.
Look at me, vibing.
6:15pm
The third one wasn't quite as easy -- they warned this one could "sting my veins".
Dacarbazine
Why I need this: Used to treat cancer of the lymph system (and interferes with the growth of cancer cells).
Fun fact: They tested this drug on rats and rabbits back in 2014. They saw that offspring of female rats had dozens of abnormalities. If I were pregnant, this drug would definitely not be safe to take.
Potential side effects:
- Redness, pain, or swelling at place of injection
- Black, tarry stools
- Blood in urine or stools
- Cough or hoarseness, accompanied by fever or chills
- Fever or chills
- Lower back or side pain, accompanied by fever or chills
- Painful or difficult urination, accompanied by fever or chills
- Pinpoint red spots on skin
- Unusual bleeding or bruising
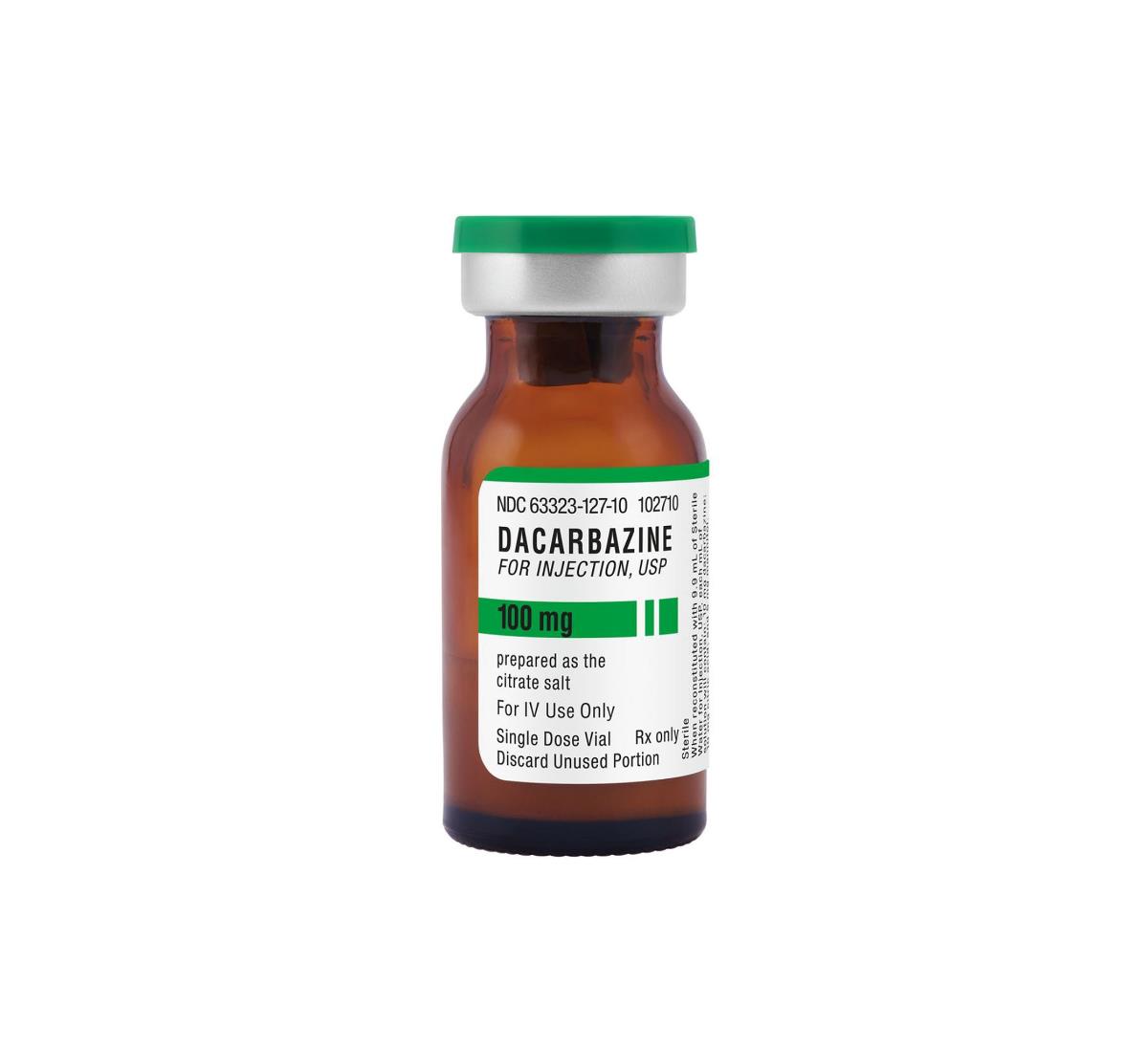
This one takes a full hour for some reason.
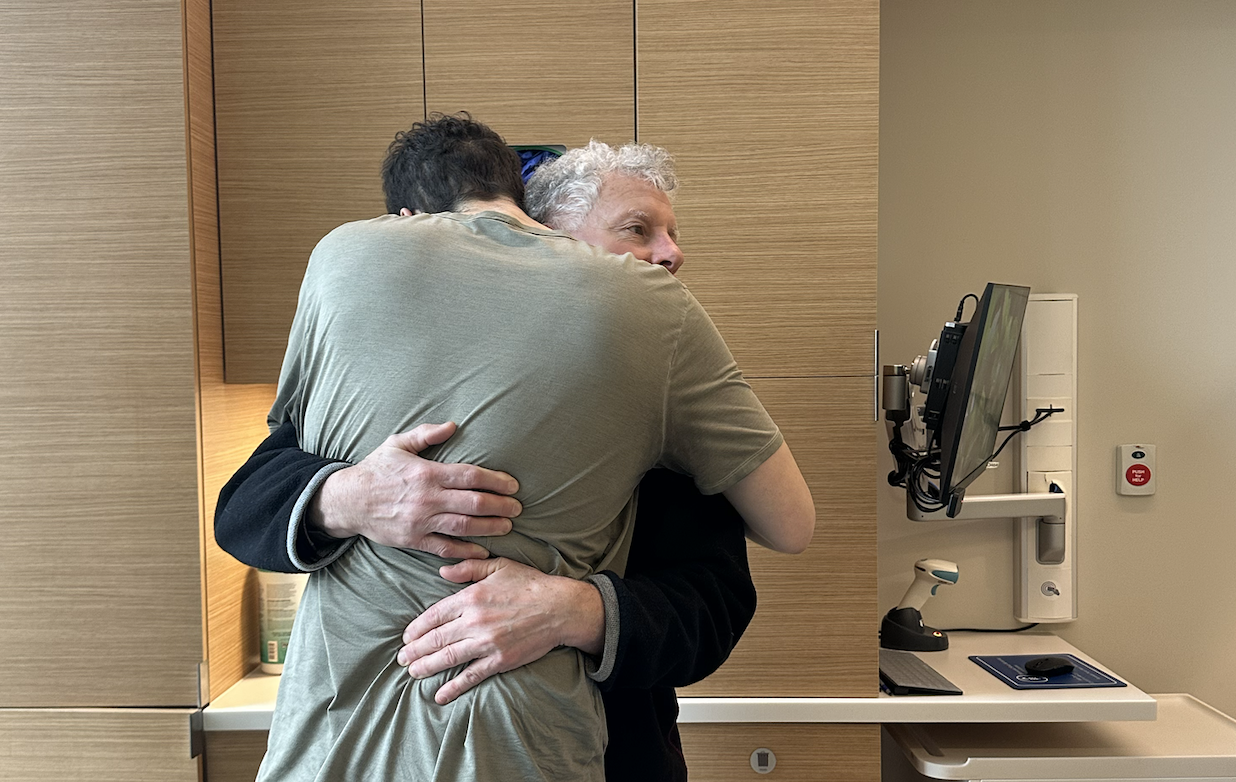
Dad and Mom needed to head out and catch their plane back to Boston.

7:30pm
The last treatment of the day was the immune therapy.
Option 1: Rituximab (approved by FDA in 1997):
- How it works: Targets the CD20 protein on B cells in lymphoma. By binding to CD20, Rituximab helps the immune system to recognize and destroy these cells.
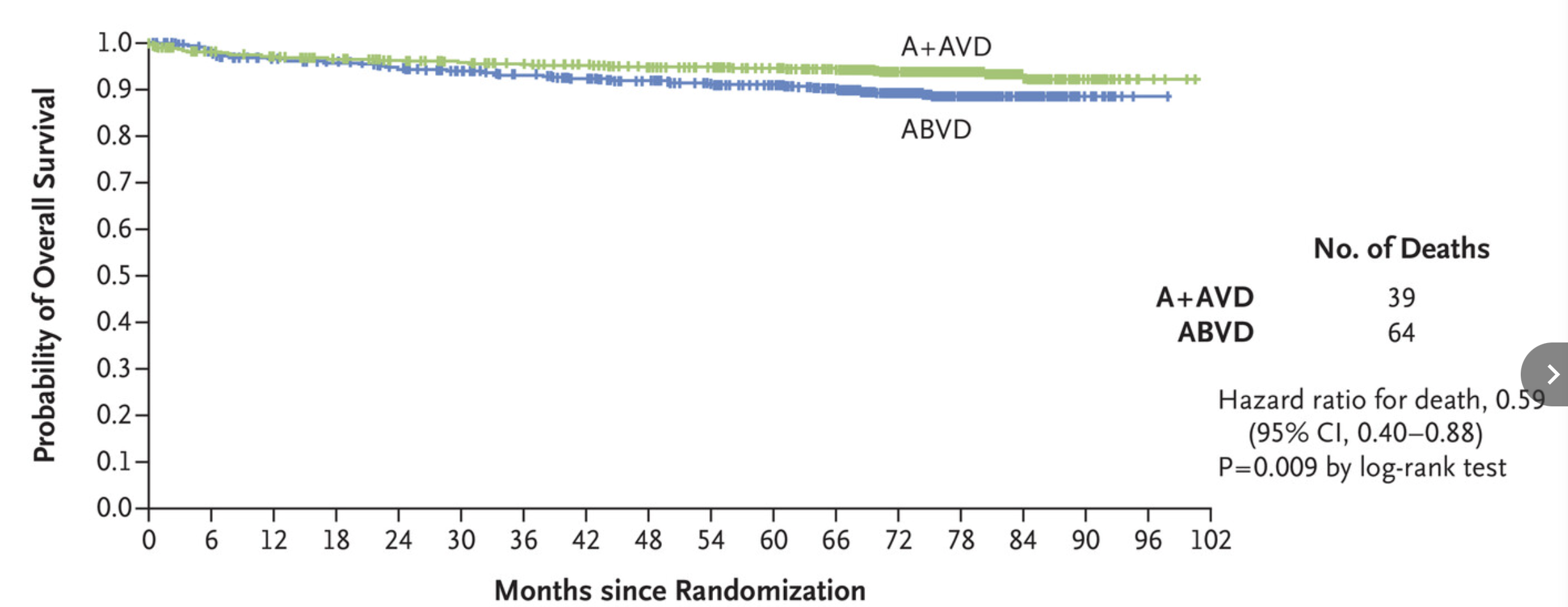
Study: Overall Survival with Brentuximab Vedotin in Stage III or IV Hodgkin's Lymphoma
- 1300 patients received 6 months of treatment.
- 664 patients got Rituximab.
- 670 patients got Brentuximab.
- Rituximab had a 89.4% 6-year overall survival estimate.
- Brentuximab had a 93.9% 6-year overall survival estimate.
Study Chart
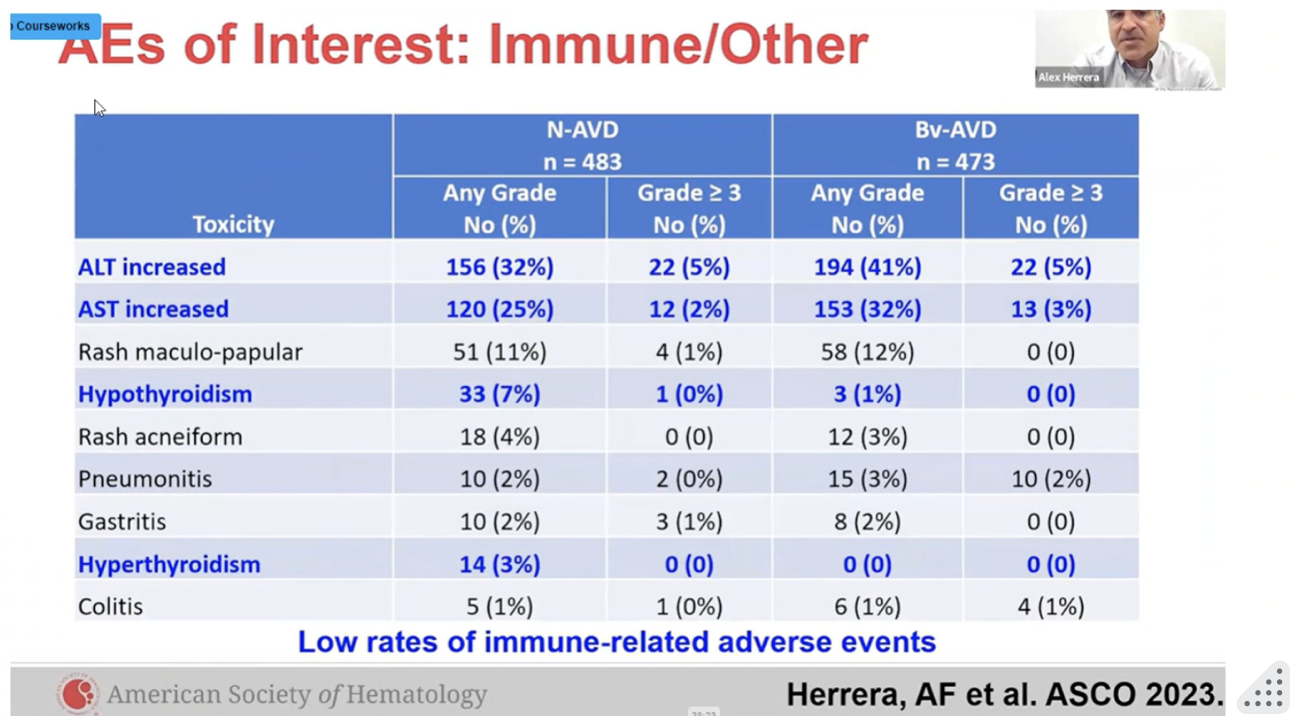
Option 2: Brentuximab (approved by FDA in 2011):
- How it works: Targets CD30, a protein on the surface of lymphoma cells. This allows more direct delivery of chemotherapy to the cancer cells, reducing the impact on healthy cells (and potentially leading to fewer side effects compared to Rituximab).
- Side Effects: It can cause some of the usual chemo side effects, like tiredness and lower blood cell counts, but it's more focused so it might be easier on you than traditional chemo.
Option 3: Nivolumab (approved by FDA in 2016):
- How it works: It blocks PD-1, a trick cancer cells use to hide from your immune system. By blocking PD-1, Nivolumab makes the cancer cells visible again, so your immune system can attack them.
- Side Effects: It can rev up your immune system too much, causing inflammation in parts of the body.
- 994 patients were enrolled from 7/9/19 to 10/5/22.
- 487 got Brentuximab.
- 489 got Nivolumab.
- 86% did not have a relapse after 1 year with Brentuximab.
- 94% did not have a relapse after 1 year with Nivolumab.
7:45pm
Time for Nivolumab.
The nurse tells me that sometimes the drug causes back pain, but it's unlikely. She starts the infusion, and tells us to click the "red button" if we need her.
She'll be back in 10.
About 30 seconds after the nurse left the room, something was off.
A moment later, the distant feeling of my heart beat turned into a sound. It became louder and louder.
Have you ever seen one of those war movies where you only hear the thumping of the person's heart? It was like that.
Then, I realized my chest was constricted. I'd try to breath in, but was cut off short.
I tell Mikayla: "Something's not right" and I hit the red button.
Fives seconds later a nurse came in, followed by another, and another. They turn off the Nivolumab.
As the drug stopped, I observed myself easing up. My face flushed and I noticed a new layer of sweat.
They check my vitals, everything was okay.
Mikayla almost had a panic attack. I thought we should check her vitals, not mine.
** photo she made me delete because "why would you take a photo of me freaking out"**
I asked if I could post this one and she said: "yeah because I'm not fucking traumatized in that one."

The nurse tells me not to worry and starts giving me Benadryl through the IV (50mg, about 2 pills worth). They warned it may hurt a bit, but they undersold this one. My veins were stinging. It felt like bees were attacking my arm.
A few seconds later, I'm yawning. It takes 30 minutes for Benadryl tablets to kick in, 5 seconds for the IV to do it's thing. I was thoroughly impressed.
They get a Doctor on the phone, and he says we're good to move forward.
They begin the Nivolumab again, this time only having it go at 25% of the previous speed. The rest was smooth sailing.
Here's my sleepy reaction to the whole thing.
After we were wrapped up, I needed to go to the bathroom.
Nothing makes you feel more sick than wheeling this thing to take a piss.

I took some mirror selfies for the memory.

Phew that was a long one! Thanks for reading through, I know this wasn't easy.
I have a handful of shoutouts to give, but will be saving those for the next updates :)
As always, I love your responses here. It makes my day to know you're keeping up and supporting along the way. Your words actually makes this whole thing far easier, so please send me your thoughts!
Love,
David